Table of Contents
What Is Hypotonia?
Hypotonia means low muscle tone. The condition first describes in 1956 among children who were called “lazy children”.
In healthy muscles, a certain amount of rigidity or tension is always maintained even at rest. It can be clinically set as muscle tone.
The tone of the abdominal muscles, for example, waits on the abdominal contents and that of the back keeps the back right and allows walking, standing etc.
The tone reduces during sleep. If a person bulldozes away, this lack of style usually leads them to fall. Hypotonia is a sick condition that results in limbs with rubber consistency that cannot stop.
Symptoms of Hypotonia
Children accentuate their spinal curve at the first look, the protruding part of their abdomen (due to lack of abdominal muscle tone).
When walking, victims have flat feet, toe walking, and difficulty walking on the heels.
In babies, there is a developmental delay, loose joints etc. In children over 8, there may be muscle contractions, muscle pain etc.
Causes of Hypotonia
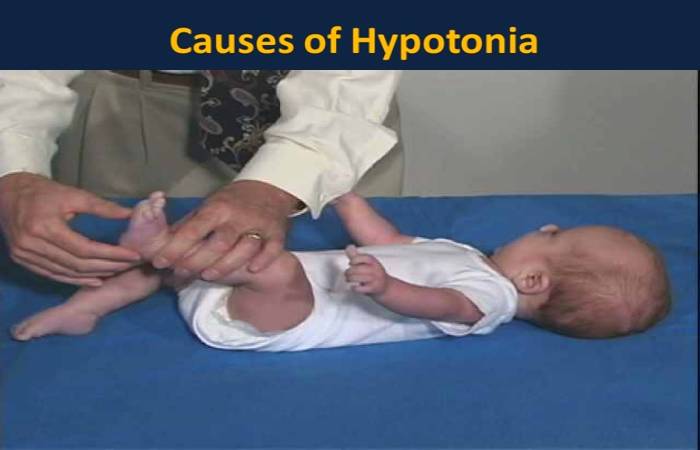
Hypotonia in a child can be due to multiple causes. Benign congenital hypotonia manifests at birth and generally appears as regular limbal movements and tendon reflexes along with weakness.
There may be mild or regular retardation in engine developments that improve with age.
In tests, the levels of muscle enzymes and results of electromyography (EMG) and nerve conduction studies, as well as muscle biopsy studies, appear normal.
Who is Affected by Hypotonia?
Affected children have a 30% chance of having someone in the family with a similar affliction. Boys and girls are equally affected.
Four different sites of hypotonia:
- The cause of the condition lies in four various areas:
- In the central nervous system (66 to 88% cases)
- In the peripheral motor and sensory nerves
- At the neuromuscular junction (the connection point the end of the nerve meets the muscle to transmit the impulse for movement and contraction of the power)
Types of Hypotonia

Hypotonia is a symptom of another underlying condition. And also, it is of two types congenital and detected.
1. Congenital Hypotonia
- It is present at birth. It is generally an inherited or genetic condition that affects the nerves, brain, or muscles.
- Some conditions that cause congenital hypotonia are Down syndrome, Marfan syndrome, dyspraxia, cerebral palsy, etc.
2. Hypotonia Detected
- Symptoms of hypotonia develop after birth as the result of an underlying medical condition, injury or trauma.
- Conditions that can lead to hypotonia include muscular dystrophy (gradual weakening and damage of the muscles), brain infections such as meningitis or encephalitis, head injury.
- And also, myasthenia gravis (an autoimmune disease where the immune system attacks healthy muscles leading to severe weakness.)
Diagnosis of Hypotonia
It is usually diagnosed at birth by the attending paediatrician. And also, a neurologist can follow it.
Treatment of Hypotonia
The treatment plan involves managing the underlying cause. Premature babies born with hypotonia can sometimes grow out of it on their own.
Those with infections can treat accordingly. However, if the underlying cause cannot treat, physical therapy, professional therapy, and speech and language therapy may be alternative options.
When to See a Doctor
It may diagnose at birth. In some cases, however, you may not notice your child’s condition until they’re older. An indicator is that your child isn’t meeting developmental milestones.
Schedule regular appointments for your child with a doctor. Be sure to mention any concerns you have about your child’s progress.
Your doctor will assess your child’s development and run tests if they have concerns. Tests may include blood tests and MRI and CT scans.
And also, if you notice sudden signs of the condition in a person of any age, seek emergency medical care.
Conclusion
The long-term outlook depends on the following:
- underlying cause
- age
- severity
- And also, muscles affected
Having it can be challenging. It’s often a lifelong condition, and your child will need to learn coping mechanisms. They may also need therapy.
However, it’s not life-threatening, except in the cases of motor neuron or cerebellar dysfunction.

